When we talk about heart disease, the first thing that often comes to mind is high cholesterol, particularly the so-called ‘bad’ low-density lipoprotein (LDL) cholesterol. It’s something we’ve all heard about at some point or another.
But let me ask you this—what if high cholesterol isn’t the full story when it comes to your heart health?
What if there’s a hidden factor, one that standard cholesterol tests don’t even pick up?
Most of us trust that a routine cholesterol test will give us a clear picture of our heart health. But here’s the reality, standard lipid panels miss some of the most critical risk factors for heart disease.

These lab numbers give you a snapshot of your lipid profile, but here’s the reality: they don’t tell the whole story when it comes to heart health.
Traditional Cholesterol Test: Why Standard Reports Aren’t Enough?
The lipid profile measures total cholesterol, LDL, HDL, and triglycerides, but they don’t tell you the full story about LDL particle size, density, or Lipoprotein(a) levels. This is where the real risk often lies. You see, LDL isn’t just one uniform type of particle; it can vary in size and density.
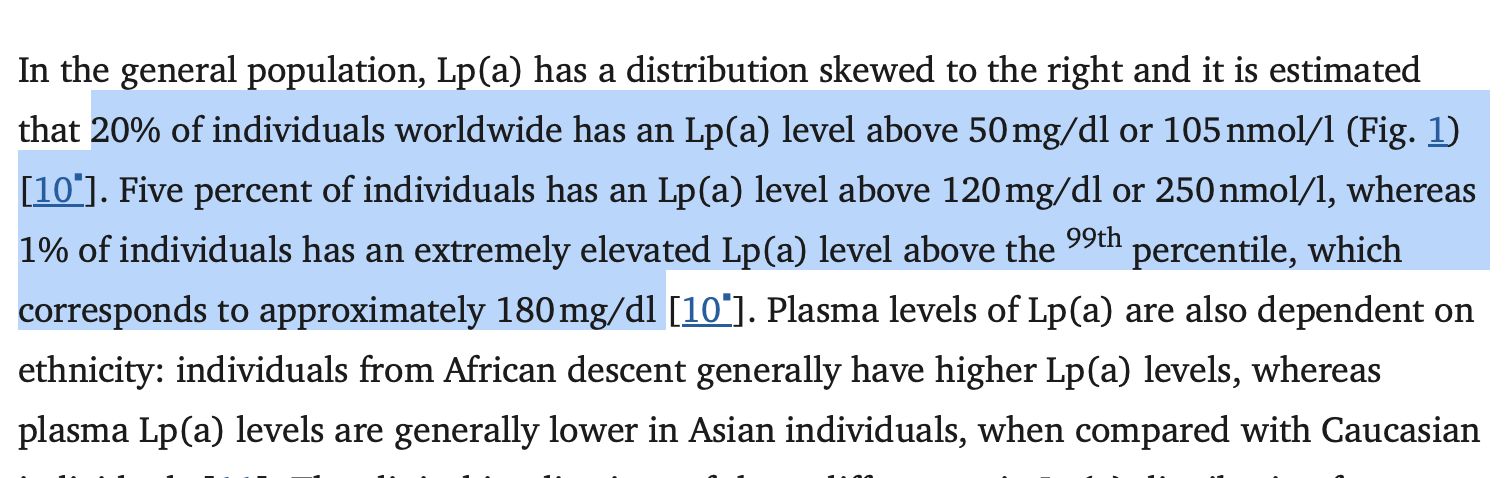
This is a huge blind spot because research shows that nearly 20-30% of the global population has elevated Lp(a) levels—a significant, independent risk factor that typical cholesterol tests don’t catch.
Now, Size Does Matter: Why Small, Dense LDL is a Bigger Problem Than You Think
You have large, buoyant LDL and small, dense LDL. While larger, buoyant LDL particles don’t pose the same risk, small, dense LDL is far more dangerous. It’s more likely to penetrate the walls of your arteries, causing plaque formation and atherosclerosis, the very conditions that lead to heart attacks and strokes.
Unfortunately, most routine cholesterol tests focus only on total LDL levels, which can give you a false sense of security. You could have a ‘normal’ LDL level, but if a large portion of your LDL is made up of small, dense particles, your heart disease risk could still be quite high.
According to the American College of Cardiology, small, dense LDL is one of the primary reasons why people with ‘normal’ cholesterol levels can still develop heart disease. They also note that some people with a genetic predisposition have a higher proportion of small, dense LDL particles, even if their total cholesterol is within range.
So, knowing the size and density of your LDL particles could be the key to understanding your real heart health risk.
This is not something you want to leave to chance, especially if you have a family history of heart disease.
Studies show that small, dense LDL particles are more atherogenic (likely to cause artery blockages) than larger particles. This is why traditional lipid profiles may not give you the full picture of your cardiovascular risk.
Lp(a) and Your Genes: The Heart Risk You Inherit, Not Earn
You’ve heard of LDL and HDL, but what about Lipoprotein(a), or Lp(a)? Unlike LDL, which fluctuates based on nutrition, exercise, and lifestyle habits, Lp(a) levels are hardwired into your DNA. If one or both of your parents had high Lp(a), there’s a 50% chance you inherited elevated levels too. This makes it one of the most powerful yet overlooked genetic risk factors for heart disease, strokes, and aortic valve calcification.
A staggering 20% of people worldwide have elevated Lp(a) levels, yet most of them have no idea because routine cholesterol tests don’t measure it.
Why This Matters Even If You’re ‘Healthy’
Lifestyle alone won’t bring down high Lp(a) levels. Lp(a) remains fairly constant throughout life. While some individuals may see marginal reductions through specific nutrition and supplement interventions, the effect is usually minimal.
This is why many people with ‘perfect’ cholesterol numbers still suffer unexpected heart attacks because their standard lipid panel didn’t catch high Lp(a). If your family has a history of early heart disease or unexplained strokes, getting tested for Lp(a) is not optional—it’s essential.
As Dr Shashank Joshi, Padma Shri Awardee & Endocrinologist puts it, “Genetics load the gun, but lifestyle pulls the trigger.” Even though your genes determine your Lp(a) levels, they don’t work in isolation; factors like nutrition, exercise, stress, and sleep play a crucial role in how these genes express themselves. While you may inherit a higher risk, the right lifestyle choices can influence whether those genes become active contributors to heart disease or remain silent. This means you have more control over your heart health than you think. Therefore, knowing your Lp(a) levels can be the wake-up call you need to take proactive steps and protect your heart before problems arise.
Because when it comes to heart disease, knowledge isn’t just power—it’s prevention.
Standard vs Advanced Cholesterol Testing: What You Need to Know
|
Test Type |
What It Measures |
What It Misses |
Why It Matters |
| Standard Cholesterol Test | Total cholesterol, LDL, HDL, triglycerides | LDL particle size, lipoprotein(a), inflammation | May overlook hidden cardiovascular risks |
| Advanced Cholesterol Test | LDL particle size, lipoprotein (a), hs-CRP (inflammation) | — | Gives a fuller picture of your heart health, especially if you have a family history of heart disease |
Importance of Advanced Cholesterol Tests
This is where it gets important for you. If you really want to assess your true risk of heart disease, you need to go beyond standard cholesterol tests. Here’s what you should be asking your doctor for:
- Lipoprotein(a) Test – This blood test measures Lp(a), which is strongly linked to heart attacks, strokes, and aortic valve disease. Standard cholesterol tests don’t measure this.
- LDL Subfraction Test – This test breaks down LDL into small, dense particles (which are harmful) and large, buoyant ones (which are relatively harmless). Standard tests only measure total LDL without differentiating between these types.
- C-Reactive Protein (CRP) Test – Measures inflammation in the body, a key driver of atherosclerosis. Chronic inflammation increases the risk of plaque buildup in the arteries, even if cholesterol levels appear normal.
If you have a family history of heart disease, or unexplained heart attacks, or want a deeper look into your cardiovascular risk, don’t wait for your doctor to bring it up, ask for these tests yourself. The more informed you are, the better you can prevent, not just treat, heart disease.
Why Aren’t These Tests More Common?
Despite their life-saving potential, these advanced tests are not part of routine check-ups.
Why?
Because most routine cholesterol tests still focus on LDL, HDL, and triglycerides only, advanced testing is often overlooked.
Traditional cholesterol testing has been the gold standard for decades, and change in medical practice takes time. Therefore, many doctors don’t routinely recommend these tests unless a patient specifically asks.
Top 3 Ways to Address High Lipoprotein(a) and Small, Dense LDL
If your Lp(a) levels or small, dense LDL particles are elevated, you might feel like you’re at the mercy of your genetics. While it’s true that you can’t change your DNA, you CAN influence how those genes express themselves—and the right lifestyle changes can help manage cholesterol more effectively than you think.
The key?
Focusing on the right lifestyle choices to reduce inflammation, support heart health, and lower your overall cardiovascular risk.
1. Eat Smart: Food for Cholesterol Management
While Lp(a) levels don’t respond significantly to food habits, addressing inflammation and oxidative stress is crucial for heart health. The best way to do this? Incorporate food for cholesterol control that’s rich in:
- Healthy Fats – Omega-3s from fatty fish, flaxseeds, and walnuts can reduce inflammation and support healthy lipid metabolism.
- Antioxidants – Colorful fruits and vegetables are packed with polyphenols and flavonoids that help fight oxidative stress, which contributes to plaque buildup.
- Nuts and Seeds – A powerful food for cholesterol control, rich in fiber and healthy fats, nuts like almonds and walnuts help manage cholesterol levels and improve heart health.
These dietary choices help reduce inflammation and support lipid metabolism, helping you manage cholesterol even if your Lp(a) levels remain unchanged.

2. Move More: Exercise as Medicine
Regular physical activity also helps manage cholesterol levels by increasing HDL and reducing small, dense LDL. Walking, strength training, and HIIT workouts don’t just burn calories, they improve your lipid profile, increase HDL (good cholesterol), and help manage blood pressure. Regular movement also enhances circulation, reducing the likelihood of LDL oxidation and plaque formation.

3. Try Smart Fasting: A Powerful Metabolic Reset
Smart fasting isn’t just about weight loss—it can play a key role in cardiovascular health. Research suggests that smart fasting may help reduce insulin levels, improve lipid metabolism, and decrease inflammation, all factors that contribute to a healthier heart.

Lifestyle Changes to Manage Cholesterol
While the top three strategies we just covered—smart nutrition, regular movement, and metabolic resets—are powerful starting points, they’re just the tip of the iceberg. True cardiovascular resilience comes from a 360-degree lifestyle shift.
To manage cholesterol and reduce the impact of genetic risk factors like lipoprotein(a), it’s essential to look beyond diet and exercise. Your daily habits, stress levels, sleep quality, and even how you breathe all influence how your body processes cholesterol and responds to inflammation.
Here’s how to build a lifestyle that actively supports your heart health, every single day:
- Prioritize Sleep: Poor sleep disrupts lipid metabolism and increases cortisol, which negatively impacts cholesterol levels.
- Manage Stress: Chronic stress elevates inflammation and contributes to arterial damage. Practices like meditation, journaling, and breathwork can help.
- Limit Smoking and Excessive Alcohol: Both can lower HDL and raise triglycerides, increasing cardiovascular risk.
- Follow Circadian Eating Patterns: Eating earlier in the day and avoiding late-night meals helps improve lipid metabolism and insulin sensitivity.
Together, these lifestyle changes help manage cholesterol effectively, even if your genetic risk is high due to elevated lipoprotein(a).
Take Charge: Your Heart, Your Responsibility
Heart disease prevention isn’t just about lowering LDL; it’s about identifying the hidden risks that most standard tests miss. Lp(a) is one of them.
If you’ve been relying solely on standard cholesterol tests to assess your heart health, it’s time to dig deeper and take a more informed, proactive approach.
The sooner you know, the sooner you can act.
WATCH ALSO
Disclaimer: This blog is for informational purposes only and is not intended to replace professional medical advice, diagnosis, or treatment. While we aim to provide accurate and up-to-date information, always consult with your healthcare provider before making any changes to your food habits, lifestyle, or medication.
Testing recommendations and treatment approaches should be discussed with a qualified healthcare professional based on your individual health profile. Your health is personal, stay informed, ask the right questions, and take proactive steps under expert guidance only.
Common Questions About Cholesterol Testing And Management
Q1. What is Lipoprotein(a), and why haven’t I heard about it before?
A: Lipoprotein(a), or Lp(a), is a genetic form of cholesterol that may increase the risk of heart disease and stroke. It’s not commonly tested because most routine cholesterol tests don’t include it.
Q2. Can lifestyle changes lower Lipoprotein(a) levels?
A: While lifestyle changes may not significantly lower Lipoprotein(a) levels directly, since this marker is largely genetic, they are crucial in reducing overall cardiovascular risk. By improving other cholesterol markers, lowering inflammation, and supporting arterial health, lifestyle choices can greatly offset the impact of elevated Lipoprotein(a), helping you protect your heart in a powerful, proactive way.
Q3. How do I know if I should get tested for Lipoprotein(a)?
A: If you have a family history of heart disease, early strokes, or heart attacks despite ‘normal’ cholesterol levels, you should request a lipoprotein(a) test from your healthcare provider.
Q4. What’s the difference between standard and advanced cholesterol tests?
A: A standard cholesterol test only gives you totals for LDL, HDL, and triglycerides. An advanced test measures lipoprotein(a), LDL particle size, and inflammation markers like CRP for a deeper look at your heart health.
Our Signature Wellness Programs integrate nutrition, breathwork, movement, stress management, quality sleep, and emotional well-being to help you build resilience against genetic predispositions.
The power to safeguard your heart is in your hands.
Take the first step today!
Schedule a one-on-one consultation with our experts by calling us at 1800 102 0253 or emailing us at consults@lukecoutinho.com.

Team Luke
Start Your Wellness Journey
Feeling inspired to take the next step in your wellness journey? Connect with us to explore how our tailored programs can support your health journey. Your transformation is just a conversation away.



