Sleeping in on weekends might feel like heaven — that cozy feeling of staying under the blanket just a little longer.
But what if you find yourself regularly sleeping more than nine hours a night? Could this be your body’s way of telling you something is off?
As I often share in my talks and videos, sleep is one of the most powerful and free medicines nature has given us. Deep, restorative sleep can regulate hormones, prime the immune system, improve mental health, and even lower your risk of chronic disease.
But too much sleep isn’t always a good thing.

Oversleeping, defined as routinely sleeping more than nine hours a night in adults, is very different from those occasional weekend catch-up sessions after a hectic week. When long sleep becomes your norm, it can sometimes point to underlying health issues.
Emerging research shows that consistently sleeping beyond nine hours is linked to a higher risk of stroke, heart disease, diabetes, obesity, depression, and even premature mortality. And that’s why we need to talk about it.
So, let’s break it down together:
- How many hours of sleep is healthy for adults
- Common reasons for oversleeping (and when to worry)
- Oversleeping side effects supported by science
- My action plan to normalize your sleep length and improve its quality
Let’s dive in!
Oversleeping Side Effects — What Research Shows
Before we explore all the risks tied to oversleeping, let’s take a minute to understand why the body regulates sleep the way it does.
Sleep Timing, Homeostasis & Sleep Disorders
Sleep timing, homeostasis, and our circadian rhythm — these are the foundations that keep us balanced.
- Sleep homeostasis is this internal drive that increases the need for sleep the longer you stay awake. Then, when you sleep, that drive dissipates. If you interrupt deep sleep cycles, or fragment your rest (for example, due to sleep apnea or frequent awakenings), your body often tries to ‘catch up’ by staying in bed longer.
- Circadian rhythms govern when we feel sleepy and when we feel alert. If these rhythms are disrupted (late nights, irregular schedules, low light during the day, too much artificial light at night), even 9+ hours may not feel restorative.
- Certain sleep disorders (like obstructive sleep apnea, restless legs, and insomnia) can severely degrade sleep quality. You may spend hours in bed, but with poor sleep architecture, the body tries to compensate by longer sleep times.
Age & Sleep Duration
Sleep needs change as we move through different life stages.
| Age Group | Recommended Sleep Duration | Why It Matters |
| Newborns (4-12 months) | 12-16 hours/day (including naps) | Crucial for brain growth, immune development, establishing sleep cycles. |
| Toddlers (1-2 yrs) | 11-14 hours/day (including naps) | Supports physical growth, learning, and emotional regulation. |
| Preschool (3-5 yrs) | 10-13 hours/day | Helps with memory consolidation, social skills, behavior. |
| School-age children (6-12 yrs) | 9-12 hours/day | Supports academic performance, growth, mental health. |
| Teenagers (13-18 yrs) | 8-10 hours/night | Balances hormonal shifts, late chronotypes, cognitive load. |
| Young Adults & Adults (18-64 yrs) | 7-9 hours/night | This is the “sweet spot” for optimal health, energy, mood, cognition. |
| Older Adults (65+ yrs) | 7-8 hours/night | Sleep often becomes lighter, more fragmented; quality is especially important. |
These underlying factors are crucial. Because some of the oversleeping side effects are not just due to duration but due to what’s happening during sleep, and what sleep you’re missing because of fragmented or poor-quality sleep.
What Science Says About Oversleeping Side Effects
Now let’s see what the research studies say about oversleeping > roughly 9 hours, especially when it happens repeatedly.
Increased Mortality Risk:
Studies found that long sleep duration (≥ 9 hours/night) was associated with about 34% higher risk of all-cause mortality compared to the reference group of 7–8 hours.
Stroke & Cardiovascular Disease Risks:
Long sleepers show a significantly elevated risk of stroke incidence and mortality. In one meta-analysis of 43 studies, long sleep (>8-9 hours) was associated with a hazard ratio (HR) ≈ 1.45 for stroke incidence and mortality, compared to ‘normal’ sleep durations.
Diabetes, Obesity & Metabolic Impacts:
Studies show that oversleeping often goes hand-in-hand with higher BMI, elevated fasting blood sugar, and risk for type 2 diabetes. In meta‐analyses, both very short and very long sleep durations are associated with worse glucose regulation.
Mood, Depression & Mental-Health Risks:
Oversleeping side effects are not limited to the body; the mind matters too. Several studies have found that sleeping too long is associated with increased risk of depression and mood disorders. Sometimes depression causes you to sleep longer, and sometimes long sleep worsens your mood. The relationship is bidirectional.
Oversleeping side effects are real, and they show up across many large, well-conducted studies. But here’s what I want you to remember:
- These studies show association, not causation. Oversleeping is often a marker — a clue that something else (a sleep disorder, metabolic dysfunction, mental health issue, poor lifestyle/circadian disruption) may be going on.
Ignoring persistent long sleep could delay diagnosing treatable conditions. Just because you’re in bed a long time doesn’t mean you’re restored.
Reasons for Oversleeping — What’s Underneath
Now let’s peel back the layers and see why oversleeping might be happening. Because oversleeping is rarely just about wanting more rest — there are real physiological, psychological, and lifestyle reasons behind it. Understanding these ‘reasons for oversleeping’ is key to knowing what to do next.
Sleep Disorders
One of the biggest reasons for oversleeping comes from poor sleep quality or fragmented sleep, which often doesn’t show up in how long you stayed in bed but in how well your brain and body got rest.
- Obstructive Sleep Apnea (OSA): Repeated pauses in breathing disrupt deep sleep. Even if you sleep 9–10 hours, you may miss restorative slow-wave or REM sleep, causing your body to try to ‘top up’ sleep. Also, there is a strong overlap between sleep apnea and hormonal/metabolic dysregulation.
- Restless Legs Syndrome/Periodic Limb Movement Disorders: Movement interruptions, often undetected by the person, can fragment sleep, pushing people into longer sleep duration to compensate. These are frequently underdiagnosed.
- Hypersomnia and Narcolepsy: In some cases, the brain’s sleep-wake regulation is altered, producing excessive sleepiness and longer nightly sleep periods. Oversleeping may be secondary to these neurological sleep disorders.
Medical & Hormonal Causes
It’s not just sleep disorders; medical issues and hormonal imbalance often show up in people who oversleep, sometimes without them realizing it.
- Hypothyroidism: When thyroid function is low, the body’s metabolism slows, leading to fatigue, sluggishness, and in many cases, increased sleep needs or a drive to remain in bed.
- Medication Side-Effects: Sedatives, antihistamines, and some antipsychotics can increase drowsiness or impair sleep architecture. Though less often the sole cause, they often amplify other issues (e.g., if someone’s sleep is already fragmented, medications can worsen the fragmentation, pushing total sleep time up).
Mental Health & Emotional Factors
Mood, stress, and mental health: they don’t just affect how you feel, they affect how you sleep — in both quantity and quality.
- Depression & Anxiety: These are strong correlates of long sleep duration. Several studies show that people with depressive symptoms often report sleeping longer.
- Emotional Burnout/Low Socioeconomic Stress: Chronic stress, burnout, or life situations that drain energy can make the body call for more rest. Also, people under high stress may have disrupted circadian rhythms, poor sleep quality, or fragmented sleep — leading to the need to spend more time in bed.
Lifestyle & Circadian Disruption
Sometimes the reasons for oversleeping are in our routines, environment, and how we treat our internal clocks.
- Irregular sleep-wake schedules/Late-night screen use: Blue light exposure at night, irregular bedtimes, or staying up late can shift circadian rhythms. Even if you go to bed ‘early,’ if your body clock is delayed or disrupted, the sleep may be less restorative, so you may sleep longer.
- Low natural light exposure: Less daylight during waking hours can weaken circadian entrainment. This can blunt the effectiveness of wake signals, so the drive to sleep remains higher.
- Chronic sleep debt/catch-up sleep: If over days or weeks, you accumulate sleep deficits, the body attempts to recover. That recovery may show up as needing extra sleep, or lingering tiredness despite ‘more sleep nights.’ But if the catch-up becomes habitual, and you’re not resolving the underlying debt or improving sleep quality, this can turn into chronic oversleep.
Remember, oversleeping is not just a habit — it’s often your body’s way of waving a red flag. Find the ‘why,’ and you’re halfway to fixing the problem.
Personalizing Your Ideal Sleep Range
Alright — this is where the ‘what works best for you’ part comes in. Science gives us ranges, but your body gives you feedback. Let’s marry both, so your sleep is optimized.
What the Research Says: 7-9 Hours Is the Sweet Spot
7–9 hours of nightly sleep is optimum for most adults when it comes to cognitive performance, mood stability, alertness, and even structural brain health.
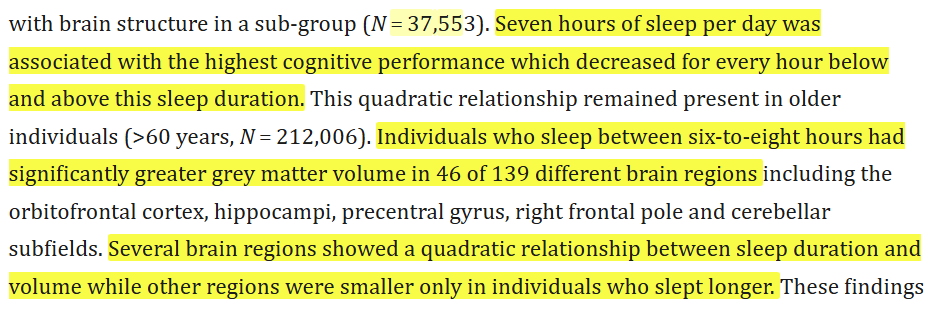
So from the studies, 7-9 hours seems to give the best balance and reduce the risk of the negative effects we discussed earlier.
What I’ve Seen in Clients & What I Teach
- I often talk about how people who think they ‘feel better with a lot of sleep’ occasionally discover that what they really need is better sleep quality (deep sleep, less fragmentation), not necessarily more hours.
- When people shift from say 10+ hours with low quality to ~8 hours of deep, continuous sleep, their energy, creativity, mood & performance often improve.
- I always encourage my community to fix their wake time first. Once wake time is consistent, your bedtime, total sleep hours, and sleep architecture tend to naturally settle.
How to Adjust Your Sleep Range Based on Personal Feedback
Here are signs to help you determine whether your personal ‘ideal’ sleep is closer to 7, 8, or even 9 hours — and when you might need more.
| Indicator | If You’re Doing Well | If You Need More or Something’s Off |
| Daytime alertness | You wake up feeling reasonably refreshed, don’t need caffeine to ‘wake up,’ maintain alertness through morning / early afternoon. | If you feel groggy, repeatedly hitting snooze, midday crashes, poor vigilance or frequent yawning. |
| Mood stability | Generally balanced mood day-to-day; manageable stress, consistent emotional energy. | If you notice irritability, low mood, anxiety creeping in, mood swings, feeling emotionally ‘flat’. |
| Cognitive performance | Good focus, memory, decision-making; able to stay on tasks, learn new things, feel mentally sharp. | Struggling with memory lapses, more mistakes, feeling foggy, slower thinking. |
| Sleep inertia/need for naps | If rare, brief; if naps are refreshing and optional. | If naps feel essential, inertia lasts long after waking, always feel you ‘slept but not rest.’ |
What If You Regularly Need More Than 9 Hours?
If you find yourself needing >9 hours for several weeks and still feeling off, these are red flags. Based on what the studies and my practice show:
- Have a sleep disorders screen (apnea, fragmentation)
- Check for medical issues (thyroid, metabolic issues)
- Assess mental health (depression, anxiety)
- Evaluate lifestyle:
- Are you consistent?
- Is your light exposure good?
- Are you using screens late?
- Are you going to bed and waking up at random times?
Putting It Into Practice: Your Sleep Calibration Steps
Here’s how I suggest calibrating your sleep to find your ideal range:
- Pick a consistent wake-up time (even on weekends) for 1-2 weeks.
- Set a sleep goal of ~8 hours — adjust bedtime accordingly.
- Keep a sleep diary. Note not just length, but how you feel upon waking, mid-morning, mid-afternoon, mood, energy.
- After 1–2 weeks, assess if you feel alert and good, that sleep is likely sufficient. If not, experiment: Shift bedtime by 15-30 mins earlier, see if quality improves.
- Don’t aim to ‘stay in bed longer’ first — aim to improve quality: light, movement, reducing disruptions or late-night screens.
Your perfect sleep number isn’t in a textbook — it’s in how refreshed, focused, and emotionally balanced you feel when you wake up.
| Area | What To Do | Why It Works |
| Daytime Anchors | Get morning sunlight within 30 mins of waking Move for 20–30 mins (walk, yoga, mobility work) Keep meal timings consistent | Light and movement reset your circadian rhythm, regulate melatonin and cortisol, and build a strong internal clock. |
| Evening Routine | Go screen-free 60–90 mins before bed Eat light, avoid late caffeine/alcohol Practice breathwork or meditation | Prepares the brain to wind down, keeps blood sugar stable, and activates the parasympathetic (rest-and-digest) system. |
| Sleep Environment | Keep bedroom cool, dark, quiet Remove screens from bed Track sleep with a diary or wearable | Signals safety and darkness to the brain, helping you fall asleep faster and stay asleep longer. Tracking helps you find your natural “sleep budget.” |
You don’t need to fix everything at once. Pick 1–2 habits from each column this week, stay consistent, and build from there. Sleep quality transforms when you layer these small changes consistently.
When to Seek Medical Help
While most cases of oversleeping can be fixed with lifestyle changes, some require medical evaluation. Please don’t ignore these red flags — they might be your body’s SOS.
- Loud snoring, choking, or gasping during sleep could indicate sleep apnea
- Morning headaches, extreme fatigue, poor focus – possible sleep-disordered breathing or hormonal imbalance
- Persistent oversleeping >3–4 weeks with no obvious reason – rule out thyroid, depression, or medication effects
- Low mood, loss of interest in daily life – screen for depression or burnout
- New neurological symptoms (weakness, confusion, memory issues) – seek urgent medical help
If your doctor suspects a sleep disorder, they might recommend a sleep study to track your brain waves, breathing, and oxygen levels overnight — you can read our detailed guide on sleep studies here.
Early evaluation saves lives. Oversleeping is often a clue, not a curse — catch the cause early, and your health trajectory can change for the better.
The Last Word
I’ve always believed that sleep is the most powerful drug we never have to pay for. But just like too little sleep can hurt us, too much sleep — or oversleeping — can also be a sign that something deeper needs our attention.
Don’t treat oversleeping as laziness. Treat it as data. Take one step today — maybe it’s morning sunlight, maybe it’s reviewing your bedtime routine, maybe it’s talking to your doctor. You’ll be surprised how quickly your sleep and your health can transform.
Frequently Asked Questions
How many hours of sleep is healthy for adults?
Most adults thrive on 7–9 hours of sleep per night. Research shows this range supports memory, immunity, and mental health. Consistently needing more may signal underlying health issues. If you wonder how many hours of sleep are healthy for you, track your alertness and mood across a few weeks.
What are the common oversleeping side effects?
Studies link oversleeping side effects to higher risks of stroke, heart disease, obesity, diabetes, and even depression. Chronic oversleeping (more than 9–10 hours) can also cause headaches, back pain, and grogginess. While oversleeping itself isn’t always the cause, it often indicates an underlying health concern that needs attention.
What are the most common reasons for oversleeping?
The top reasons for oversleeping include sleep apnea, narcolepsy, hypothyroidism, depression, chronic fatigue, medication side effects, and poor circadian rhythm due to late-night screen use or irregular schedules. Identifying the root cause with a doctor or sleep specialist is key to restoring healthy and refreshing sleep patterns.
Can oversleeping affect mental health?
Yes. Oversleeping and mental health have a two-way relationship. Excessive sleep can worsen symptoms of depression and anxiety, while mood disorders can make you sleep longer. Addressing both — through therapy, routine, and lifestyle — often improves energy levels and emotional resilience over time.
When should I seek medical help for oversleeping?
Seek help if oversleeping lasts over 3–4 weeks, causes fatigue, poor focus, or mood changes, or if you experience loud snoring, morning headaches, or choking during sleep. A doctor can rule out medical conditions and help personalize your sleep range for optimal health and longevity.
Disclaimer: This blog is for educational and informational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or qualified healthcare provider with any questions you may have regarding a medical condition or sleep disorder.
If you’re struggling with sleep or chronic fatigue, don’t wait.
Set up a one-on-one consultation with our integrative team or explore our Wellness Programs to optimize your sleep.
Reach out to us at 1800 102 0253 or write to us at consults@lukecoutinho.com.

Team Luke
Start Your Wellness Journey
Feeling inspired to take the next step in your wellness journey? Connect with us to explore how our tailored programs can support your health journey. Your transformation is just a conversation away.



