Living away from home; whether you’re a student in a hostel, a young professional juggling deadlines, or someone constantly on the move, can make it challenging to maintain a balanced food habit. Skipped meals, reliance on packaged food, and irregular eating habits are more common than we think, and over time, these patterns can silently affect our health. One of the key areas impacted is our hemoglobin levels.
Understanding Hemoglobin
Hemoglobin is the molecule that gives your blood its rich red color and your body the energy to function. Every time you take a breath, hemoglobin becomes the carrier that transports oxygen from your lungs to every single cell in your body and returns with carbon dioxide for exhalation; a beautiful cycle that keeps you alive, alert, and energized.

When your hemoglobin levels dip, oxygen transport slows down, and the body’s cells are left slightly ‘oxygen-starved.’ This is why fatigue, weakness, or breathlessness often appear even before your lab reports confirm a deficiency. It’s not just about the numbers on a blood test, it’s about how efficiently your body can deliver energy to every organ, muscle, and tissue.
| Interestingly, hemoglobin in women tends to fluctuate more than hemoglobin in men due to menstrual blood loss, pregnancy demands, and hormonal changes. In contrast, men typically have higher baseline levels because testosterone stimulates red blood cell production, a natural physiological advantage. |
But despite these gender-based differences, the principles of supporting hemoglobin remain the same: nourish, rebuild, and maintain balance through mindful nutrition and lifestyle choices.
So before you jump straight to the list of foods for increasing blood levels, pause to know the reasons why your hemoglobin is low in the first place.
Causes of Low Hemoglobin
Let’s explore the causes that can deplete this vital oxygen-carrying protein in your blood.
1. Nutritional Deficiencies:
Your body depends on a steady supply of specific nutrients to make hemoglobin, primarily iron, vitamin B12, and folate.
Iron forms the core of hemoglobin; without it, your red blood cells can’t carry oxygen effectively. The World Health Organization identifies iron deficiency as the leading global cause of anemia, especially among women of reproductive age.

- Vitamin B12 and Folate are equally critical for red blood cell formation and DNA synthesis. Deficiencies in these vitamins can reduce both the size and number of red blood cells, leading to fatigue, weakness, and neurological symptoms.
2. Blood Loss:
Chronic or excessive blood loss drains your body’s iron reserves faster than it can replenish them.
- Heavy menstrual cycles are a major contributor for fluctuating hemoglobin in women.
- Other sources of blood loss, such as gastrointestinal bleeding from ulcers or long-term use of painkillers (NSAIDs), can also silently reduce hemoglobin levels without immediate symptoms.

3. Chronic Health Conditions:
Sometimes, low hemoglobin isn’t about nutrition or blood loss at all, it’s a byproduct of an ongoing medical condition.
- Kidney disease reduces the production of erythropoietin, a hormone that signals your bone marrow to make red blood cells.
- Thyroid disorders and autoimmune inflammation can suppress red blood cell synthesis by altering metabolism and immune function.
4. Genetic Factors: When It Runs in the Family
Certain genetic conditions, like thalassemia or sickle cell anemia, affect hemoglobin structure or production. These inherited traits alter how oxygen is transported, making management more complex. While genetics can’t be changed, lifestyle and nutrition, including the right food to increase blood level, can significantly support quality of life and reduce complications.
5. Lifestyle Habits:
In today’s fast-paced world, hemoglobin health often takes a backseat to convenience.
- Skipping meals, surviving on processed food, late-night work, and constant stress all deplete the body’s nutrient reserves and impair iron absorption.
- Chronic stress also raises cortisol, which interferes with red blood cell production.
- Poor sleep adds to the problem as irregular sleep patterns can alter inflammatory and hormonal pathways linked to red blood cell synthesis.
A Common Misconception: Low hemoglobin doesn’t always mean you need to ‘fix your blood’, it often points to what your body has been deprived of. For hemoglobin in women, the underlying issue could be hormonal imbalance or inadequate nutrition during menstruation or pregnancy. For hemoglobin in men, it could relate to poor dietary diversity or lifestyle stressors. Addressing the ‘why’ behind the low numbers allows you to correct it from the inside out, not just the lab report level.
Symptoms to Watch For
Here’s what to look out for:
1. Persistent Fatigue and Weakness
This is often the first red flag. Low hemoglobin means your red blood cells carry less oxygen to muscles and tissues. As a result, your body struggles to generate energy efficiently. Even mild anemia significantly reduces physical endurance, cognitive alertness, and overall wellness.
2. Dizziness, Headaches, or Lightheadedness
Feeling dizzy when you stand up quickly or climb stairs?
That’s often due to reduced oxygen delivery to the brain. Low hemoglobin compromises cerebral oxygenation, affecting concentration and balance. Chronic low hemoglobin levels can impair cerebral blood flow and trigger headaches or fainting spells, especially in hemoglobin in women during menstruation or pregnancy.
3. Pale Skin, Lips, or Nail Beds
Paleness is your body’s visual warning system. When hemoglobin levels fall, the bright red hue of oxygen-rich blood fades, leaving your skin, lips, or even nail beds looking unusually pale. Changes in nail color and brittleness are among the earliest non-invasive indicators of iron deficiency.
4. Shortness of Breath or Rapid Heartbeat
Low hemoglobin forces your heart to work harder to compensate for the reduced oxygen-carrying capacity of your blood. This can lead to palpitations, shortness of breath, or a feeling of ‘racing heart’ even with light activity.
Anemia increases cardiac output and respiratory rate to maintain oxygen supply, putting extra strain on the heart, especially concerning hemoglobin in men, who may experience these symptoms without realizing they stem from low iron or B12 levels.
5. Cold Hands and Feet or Numbness
When blood is low in hemoglobin, your body prioritizes oxygen delivery to vital organs; the brain and heart, over the extremities. That’s why cold hands and feet, tingling, or numbness can be subtle signs that your blood oxygen transport is compromised.
6. Mood Changes and Brain Fog
Low hemoglobin affects more than just energy; it influences emotional and mental well-being too. Insufficient oxygen supply to the brain can trigger irritability, poor focus, and even mild depressive symptoms. In fact, anemia is linked to neurotransmitter imbalance, showing that iron and B12 deficiencies alter serotonin and dopamine metabolism, two key mood-regulating chemicals.
7. Brittle Hair or Hair Fall
Your hair follicles are highly sensitive to oxygen supply. When hemoglobin levels drop, your body diverts oxygen away from non-essential functions like hair growth to sustain vital organs. Over time, this leads to dull, dry, or thinning hair.

How Low Hemoglobin Is Diagnosed
Before jumping to supplements or remedies, the most important step is understanding what your blood is really trying to tell you. Low hemoglobin isn’t a standalone condition; it’s a sign that your body needs attention, nourishment, or sometimes deeper medical evaluation.
Diagnosis begins with a simple blood test — the Complete Blood Count (CBC).
This test measures your hemoglobin, hematocrit (the percentage of red blood cells in your blood), and red blood cell indices MCV (Mean Corpuscular Volume), MCH (Mean Corpuscular Hemoglobin), and MCHC (Mean Corpuscular Hemoglobin Concentration), which help your doctor understand the type and possible cause of anemia.
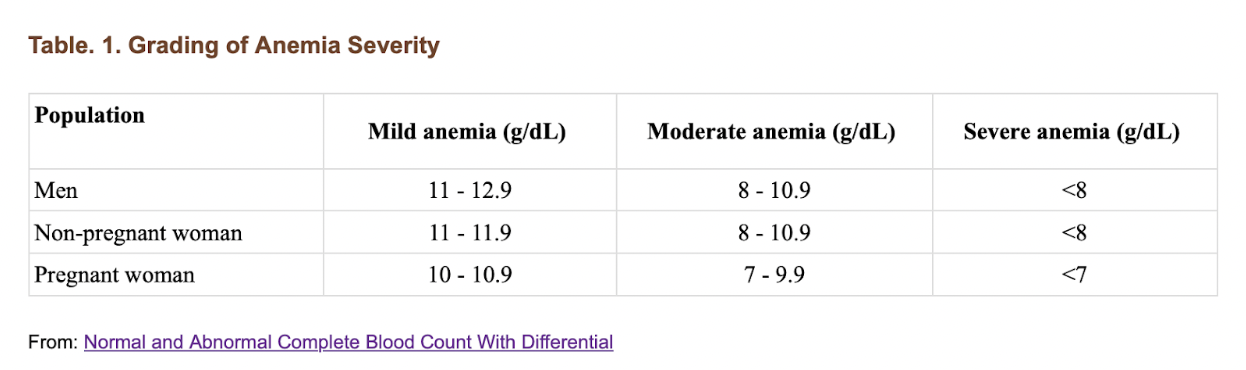
Here’s what doctors usually look at:
- Hemoglobin (Hb): Measures how much oxygen-carrying protein is in your red blood cells.
- Normal range:
- Men: 13 to 18 g/dL
- Women: 12 to 16 g/dL
- Normal range:

- Hematocrit (Hct): Reflects the proportion of red blood cells in your blood. Low values confirm that your blood has fewer cells to carry oxygen.
- Red Blood Cell (RBC) Indices:
- MCV (Mean Corpuscular Volume): Tells whether your red blood cells are small (microcytic, often due to iron deficiency) or large (macrocytic, often due to B12 or folate deficiency).
-
- MCH & MCHC: Indicate how much hemoglobin each red cell contains.
Once anemia is confirmed, your doctor may order additional tests to pinpoint the root cause:
- Serum Ferritin and Iron Studies: To check your iron stores and absorption capacity.
- Vitamin B12 and Folate Levels: Deficiencies here can cause megaloblastic (large-cell) anemia.
- Reticulocyte Count: Measures how quickly your bone marrow is producing new red blood cells.
- Liver and Kidney Function Tests: To rule out organ-related causes of low hemoglobin.
- Thyroid Profile: Since hypothyroidism can also contribute to fatigue and low red cell production.
- Stool Occult Blood Test or Endoscopy: If internal bleeding is suspected.
In women, menstrual history and dietary assessment are equally important. In men and postmenopausal women, unexplained anemia often prompts further evaluation for gastrointestinal issues or chronic disease.
Top Foods to Increase Hemoglobin Naturally
When it comes to increasing hemoglobin, food isn’t just fuel, it’s information. Every bite communicates with your cells, influencing how efficiently your body produces red blood cells and carries oxygen. While supplements can play a role in medical deficiencies, only if it is prescribed by your doctor, your daily meals remain the most sustainable and natural way to increase hemoglobin over time.
Iron, vitamin B12, folate, and vitamin C all contribute to the complex yet beautifully coordinated process of red blood cell formation. So rather than chasing just one nutrient, it’s about creating balance on your plate.
Let’s explore the most effective food categories and how to make them work for you.
1. Iron-Rich Foods
Iron forms the very backbone of hemoglobin. There are two types of dietary iron; heme iron (from animal foods) and non-heme iron (from plant foods). Heme iron is absorbed more efficiently, but with the right combinations, plant-based sources can be just as powerful.
- Plant Sources: Spinach, kale, amaranth leaves, moringa, jaggery, lentils, chickpeas, and tofu. Non-heme iron absorption can vary, therefore, combining these foods with vitamin C sources significantly increases uptake.
- Animal Sources: Lean red meat, chicken liver, eggs, and fish like sardines or mackerel are highly bioavailable sources of heme iron.

Pro Tip: Always cook leafy greens lightly, overcooking destroys some of their nutrient content. And when possible, pair your iron-rich meal with lemon, tomatoes, or bell peppers for enhanced absorption.
2. Vitamin C-Rich Foods
Vitamin C acts as a natural enhancer of iron absorption by converting ferric iron (Fe³⁺) into its more absorbable ferrous form (Fe²⁺). In simpler terms, it’s your body’s way of unlocking the full potential of the iron you eat.
Best Sources: Citrus fruits, guava, bell peppers, amla, strawberries, and kiwi.
Co-consumption of just 75–100 mg of vitamin C can increase non-heme iron absorption by up to four times.
Try adding freshly squeezed lemon to your spinach dal or snacking on guava after a meal. It’s a simple, natural, and delicious way to enhance your food to increase blood level without any supplements.

3. Folate and Vitamin B12 Sources
Your red blood cells can’t form or mature properly without adequate folate and vitamin B12. Folate (vitamin B9) helps in DNA synthesis during red blood cell production, while vitamin B12 supports hemoglobin’s structure and function. Deficiency in either can lead to megaloblastic anemia, where cells are large but ineffective in oxygen transport.
- Folate-Rich Foods: Lentils, chickpeas, black beans, green peas, and dark leafy greens.
- Vitamin B12 Sources: Dairy products, eggs, fish, fortified plant milks, and nutritional yeast.
Even marginal deficiencies in B12 or folate can impair erythropoiesis (RBC production). This is particularly relevant for hemoglobin in men and hemoglobin in women following vegetarian or vegan diets where B12 intake may be low.
Practical Tip: If you’re vegetarian, consider fortified cereals, plant-based milks, or a healthcare-supervised B12 supplement.
4. Other Supportive Foods
Sometimes, the smaller players make a big difference. Several foods act as natural enhancers to maintain overall hemoglobin levels by supporting liver function, antioxidant defense, and blood purification.
- Nuts and Seeds: Pumpkin seeds, sunflower seeds, and almonds provide zinc and copper; cofactors essential for iron metabolism.
- Beetroot and Pomegranate: These foods don’t just ‘color your blood’, they support nitric oxide production and vascular health, indirectly enhancing oxygen utilization. Regular beetroot juice consumption improved hemoglobin levels and reduced fatigue in mildly anemic women.
Try Luke’s Heart Beet Blast: One Simple Drink to Support Your Blood Vessels and Heart Health
- Dates and Raisins: Rich in natural iron and easy to digest, they can serve as a mid-day snack that supports food for increased blood level.
Pro Tip: Pair iron-rich nuts or seeds with a fruit high in vitamin C for better iron assimilation, for example, a handful of pumpkin seeds with orange slices.
Note: While these foods are powerful, remember that not every food suits every individual. People with certain conditions; such as thalassemia, hemochromatosis, or kidney disorders, must be cautious with iron intake. Always consult a qualified healthcare professional before making significant changes in food habits.
Low hemoglobin is often a symptom, not the root cause. For some, especially women with heavy menstrual cycles or underlying hormonal imbalances, the solution isn’t just about iron-rich meals but understanding the body’s deeper signals and needs.
Food is medicine, but only when chosen mindfully, paired correctly, and aligned with your unique physiology.
Lifestyle Practices for Healthy Hemoglobin
Optimizing hemoglobin isn’t just about what you eat; it’s about how you live. Lifestyle choices too, ensures your hemoglobin functions at its best.
Here’s how to support your blood naturally:
1. Stress Management: Meditation, Yoga, and Mindfulness
Chronic stress triggers cortisol release, which can interfere with iron metabolism and red blood cell production. Practicing meditation, yoga, or deep-breathing exercises helps regulate hormonal balance, reduces inflammation, and supports healthy erythropoiesis.
2. Moderate Exercise to Support Circulation
Exercise is a natural stimulus for blood health. Aerobic activities; such as brisk walking, swimming, or cycling, improve circulation, enhance oxygen delivery, and stimulate red blood cell production. Just a moderate, regular exercise increases erythropoietin secretion, thereby boosting hemoglobin levels, particularly in adults with borderline low hemoglobin.
Pro Tip: Avoid extreme endurance activities without proper nutrition, as overtraining can temporarily lower hemoglobin through plasma volume expansion.
3. Quality Sleep: Cellular Recharge for Red Blood Cells
Red blood cell production peaks during the night, especially in the deep stages of sleep. Consistent, restorative sleep supports immune function, hormonal balance, and red blood cell turnover, creating an optimal environment for healthy hemoglobin.
4. Avoid Smoking and Excessive Alcohol
Both smoking and heavy alcohol intake disrupt oxygen transport and can interfere with iron metabolism. Smoking increases oxidative stress, which damages red blood cells, while chronic alcohol consumption reduces serum ferritin and vitamin B12 levels, contributing to anemia and low oxygen-carrying capacity.
Therefore, abstaining from alcohol and smoking will help improve the hemoglobin levels.
Can I Take Supplements for Low Hemoglobin?
When you discover low hemoglobin levels, it’s tempting to immediately reach for an iron tablet or multivitamin. But hemoglobin isn’t just about popping an iron pill, it’s about understanding why your levels are low in the first place.
Low hemoglobin can result from several factors, like iron deficiency, poor vitamin B12 or folate intake, chronic inflammation, poor gut absorption, menstrual blood loss, or even hidden internal bleeding. So before beginning any supplement, the golden rule is: test, don’t guess.
Your doctor can identify what’s really driving the low hemoglobin and guide your supplementation safely, because excess iron or B12 taken unnecessarily can be just as harmful as a deficiency.
What Doctors Typically Prescribe
If your blood tests confirm iron deficiency anemia (low hemoglobin with low ferritin), your doctor may start you on oral iron therapy; usually ferrous sulfate, ferrous fumarate, or ferrous gluconate. These are the most common and effective formulations to rebuild iron stores and improve hemoglobin.
In cases where anemia is caused by vitamin B12 or folate deficiency, supplements such as methylcobalamin (B12) or folic acid are prescribed. In some cases, B12 injections are used for better absorption, especially when gut issues or intrinsic factor deficiency are suspected.
Precautions While Taking Hemoglobin-Boosting Supplements
- Dosage:
Never self-prescribe. Over-supplementation, especially with iron, can lead to oxidative stress, liver damage, and long-term complications. Always follow the dosage your doctor recommends. - Timing:
Iron is absorbed best on an empty stomach, about one hour before meals. However, if it causes nausea or stomach discomfort, it can be taken with a small portion of food for better tolerance. - Nutrient Pairing:
Pair iron with vitamin C-rich foods like amla, citrus fruits, or bell peppers, they enhance absorption. Avoid taking it with calcium-rich foods, tea, coffee, or antacids, as they can block absorption. - Side Effects:
Iron supplements may cause constipation, bloating, or dark stools. Drink plenty of water, eat fiber-rich foods, and include healthy fats to keep digestion smooth. - Duration:
Even when your hemoglobin normalizes, continue supplements for a few months under medical guidance to rebuild iron stores completely. Stopping too early is a common reason for relapse.
Who Should Be Cautious & When to Seek a Doctor’s Help
Certain individuals need to be extra cautious before starting any iron or hemoglobin-boosting supplement:
- People with chronic diseases such as liver disorders, hemochromatosis, or thalassemia, where iron can accumulate and cause toxicity.
- Men and postmenopausal women, since their risk of iron deficiency is lower, and unnecessary supplementation can increase oxidative stress.
- Individuals with gut issues such as ulcers, gastritis, inflammatory bowel disease (IBD), or celiac disease, where absorption and tolerance vary.
- Pregnant women, who often need additional iron but in individualized doses. Over-supplementation without monitoring can increase oxidative stress or cause digestive discomfort, while under-supplementation may affect fetal development. Always follow your gynecologist’s prescribed dosage.
- Those already taking medications like antacids, thyroid medication, or antibiotics, as these can interfere with iron absorption or react with supplements.
Seek medical help immediately if you experience:
- Persistent fatigue, dizziness, or breathlessness despite supplementation.
- Blood in stool, heavy menstrual bleeding, or unexplained bruising.
- Severe abdominal pain, vomiting, or black/tarry stools while taking iron.
- A rapid drop in hemoglobin without clear cause, which could signal internal bleeding or another underlying condition.
Let’s Bust Some Myths About Hemoglobin
Myth 1: Only women need to worry about hemoglobin levels.
Fact: While it’s true that hemoglobin in women tends to be lower than men due to menstrual blood loss, men are not immune to low Hb. Poor nutrition, chronic illnesses like kidney disease or thyroid disorders, and even genetic conditions such as thalassemia or sickle cell trait can reduce hemoglobin in men.
Myth 2: Eating more red meat is the only way to increase hemoglobin.
Fact: Heme iron from red meat is highly bioavailable, but it’s far from the only solution. Non-heme iron from plant sources like spinach, lentils, beans, and pumpkin seeds can effectively support hemoglobin synthesis when combined with vitamin C-rich foods. Pairing a bowl of lentils with bell peppers or guava can enhance iron absorption as much as including a serving of meat. The key is balance and variety, not over-reliance on a single food. Incorporating diverse foods into your plate ensures sustained improvements in hemoglobin.
Myth 3: Low hemoglobin always means anemia.
Fact: Low hemoglobin is a signal, not a diagnosis. Temporary decreases can occur due to mild dehydration, acute blood loss, or short-term dietary changes. For example, women with heavy periods may experience lower Hb, but it may not indicate true iron-deficiency anemia, it could be a reflection of ongoing menstrual blood loss or hormonal imbalances. Men, too, can have transient low Hb due to high-intensity exercise or illness without meeting anemia criteria. Proper evaluation, including serum ferritin, vitamin B12, folate, and complete blood count, is essential to determine the underlying cause before labeling it anemia.
Empower Your Blood, Empower Your Life
Your hemoglobin is more than just a number on a lab report, it’s a reflection of how well your body can fuel life. The journey to healthy hemoglobin isn’t about quick fixes or chasing isolated nutrients. It’s about creating a holistic rhythm: mindful nutrition with the right food for increasing blood levels, supportive lifestyle habits, regular monitoring, and understanding your body’s unique signals.
Disclaimer: The information provided in this blog is intended for educational and informational purposes only and is NOT a substitute for professional medical advice, diagnosis, or treatment. Individual nutritional needs and health conditions vary, and what works for one person may not be suitable for another. It is important to consult a qualified healthcare professional before making significant changes to your food habits, starting supplements, or addressing symptoms such as fatigue, dizziness, or unusually low hemoglobin.
Feeling drained, dealing with hair fall, or suspecting low hemoglobin?
You don’t have to figure it out alone. Our team can help you identify the root causes and guide you with personalized nutrition, lifestyle, and medical expertise.
Set up a one-on-one consultation with our integrative team or explore our Wellness Programs.
Call us at 1800 102 0253 or write to us at consults@lukecoutinho.com to learn more.

Team Luke
Start Your Wellness Journey
Feeling inspired to take the next step in your wellness journey? Connect with us to explore how our tailored programs can support your health journey. Your transformation is just a conversation away.



